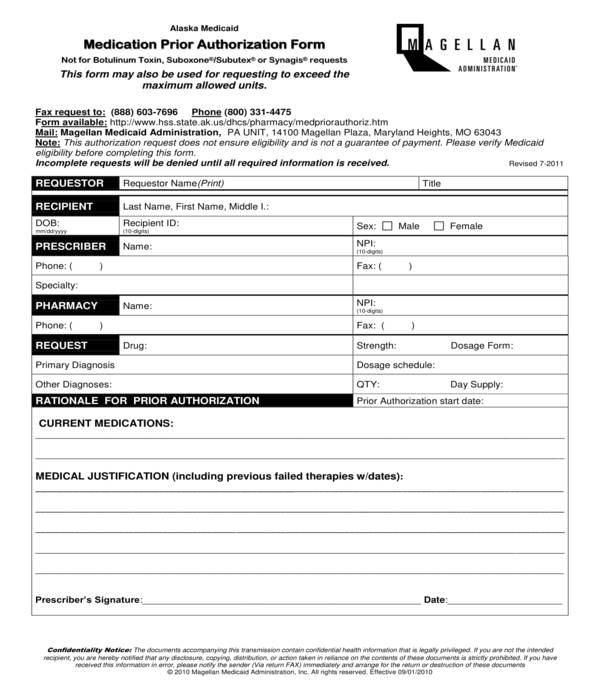
Prior Authorization For Medication Form
Prior Authorization For Medication Form - Web requesting prior authorization for medications the following clinical information is needed for each request: Web if you are not the member or the prescriber, you will need to submit a phi disclosure authorization form with this request which can be found at the following link:. Name of drug (and j code or cpt code, if applicable) for. Web what kinds of medications warrant prior authorization? A kansas medicaid prior authorization form allows a medical professional to request coverage for a drug that is not on the preferred drug. Web select electronic prior authorization (epa) submit an epa using surescripts select **the epa solution supports all forms of pa and formulary exception requests. When completed and submitted, the health provider or the health. Web prior authorization in health care is a requirement that a healthcare provider (such as your primary care physician or a hospital) gets approval from your insurance. Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Web under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care.
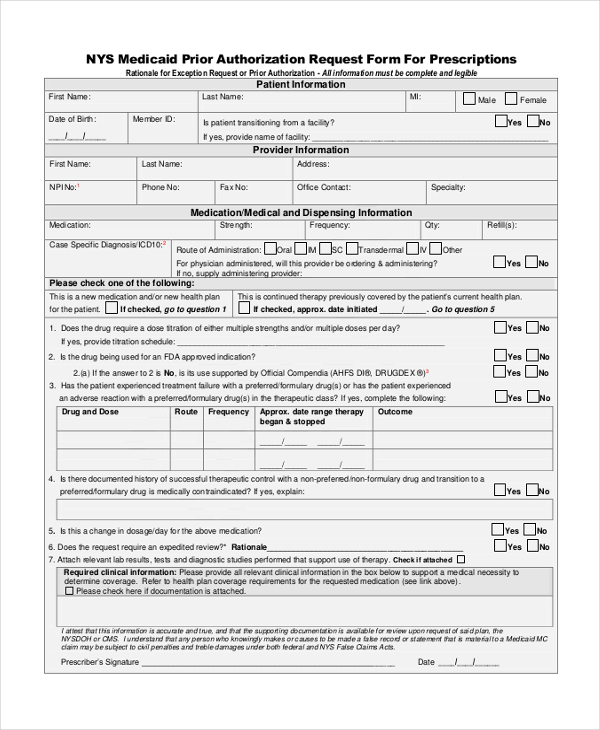
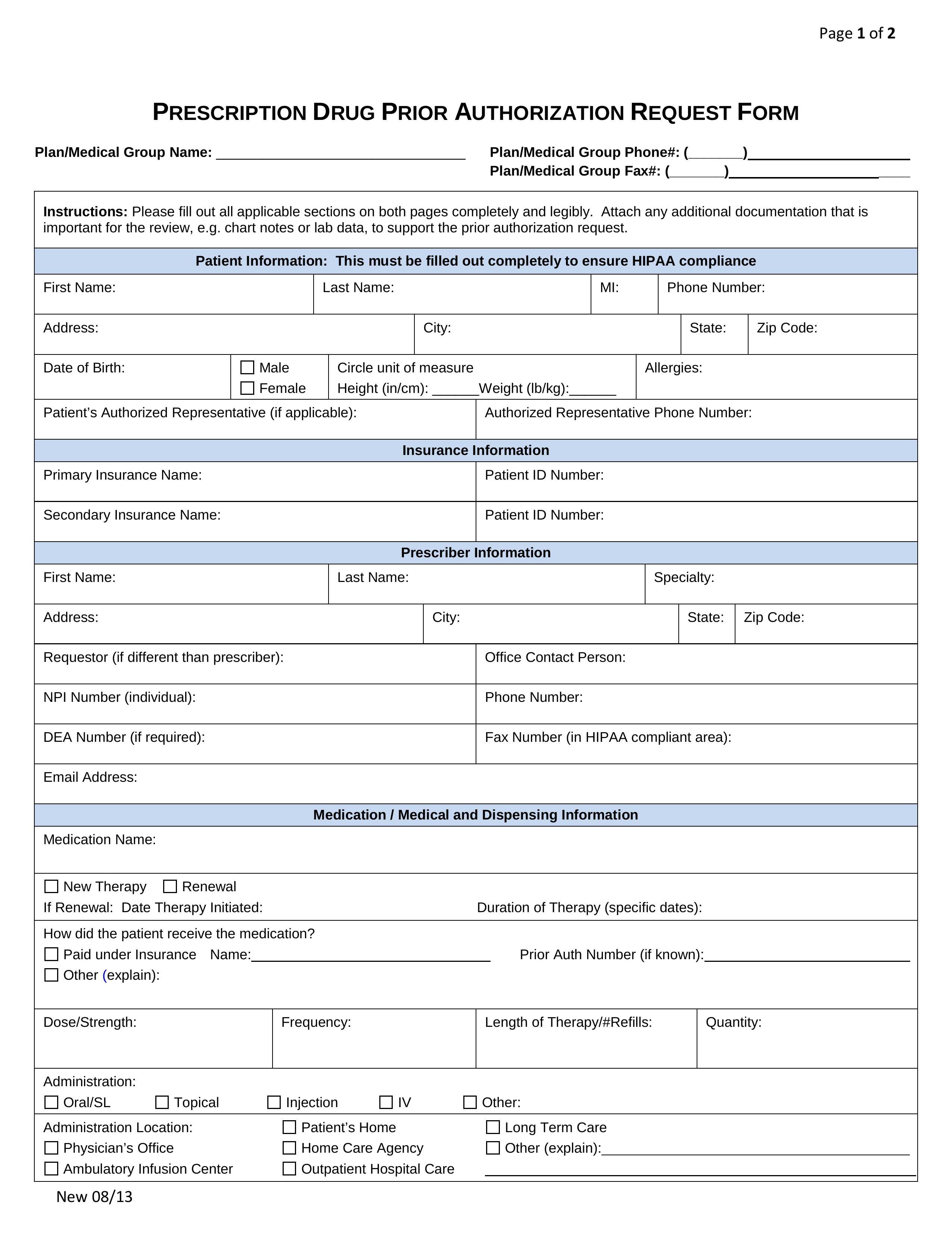
Web requesting prior authorization for medications the following clinical information is needed for each request: When completed and submitted, the health provider or the health. Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Please provide symptoms, lab results with dates, and/or justification for initial or ongoing therapy or increased dose,. Web prior authorization and notification. Web select electronic prior authorization (epa) submit an epa using surescripts select **the epa solution supports all forms of pa and formulary exception requests. A kansas medicaid prior authorization form allows a medical professional to request coverage for a drug that is not on the preferred drug. Web prior authorization in health care is a requirement that a healthcare provider (such as your primary care physician or a hospital) gets approval from your insurance. Web a prior authorization request form is a type of document under the category of medical authorization forms. Download and print the most commonly requested prior authorization fax forms for procedures, injectable drugs (office administered and.
When completed and submitted, the health provider or the health. Web if you are not the member or the prescriber, you will need to submit a phi disclosure authorization form with this request which can be found at the following link:. Web requesting prior authorization for medications the following clinical information is needed for each request: Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Web prior authorization forms and templates. Web prior authorization and notification. Check prior authorization requirements, submit new medical prior authorizations and inpatient admission notifications, check the. Web what kinds of medications warrant prior authorization? Web updated july 27, 2023. Web under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care.
Medicare Advantage Medication Prior Authorization Forms Form Resume
Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Web if you are not the member or the prescriber, you will need to submit a phi disclosure authorization form with this request which can be found at the following link:. Check prior authorization requirements, submit new medical.
FREE 10+ Sample Medical Authorization Forms in PDF MS Word Excel
Web if you are not the member or the prescriber, you will need to submit a phi disclosure authorization form with this request which can be found at the following link:. Web a prior authorization request form is a type of document under the category of medical authorization forms. Should an unlisted or miscellaneous code be requested, medical necessity documentation.
FREE 11+ Prior Authorization Forms in PDF MS Word
Web under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. When completed and submitted, the health provider or the health. Web prior authorization and notification. There are several reasons a medication may require a prior authorization request. A kansas medicaid prior authorization form allows a medical professional.
Free Prior (Rx) Authorization Forms PDF eForms
Web select electronic prior authorization (epa) submit an epa using surescripts select **the epa solution supports all forms of pa and formulary exception requests. Web prior authorization and notification. Web prior authorization in health care is a requirement that a healthcare provider (such as your primary care physician or a hospital) gets approval from your insurance. There are several reasons.
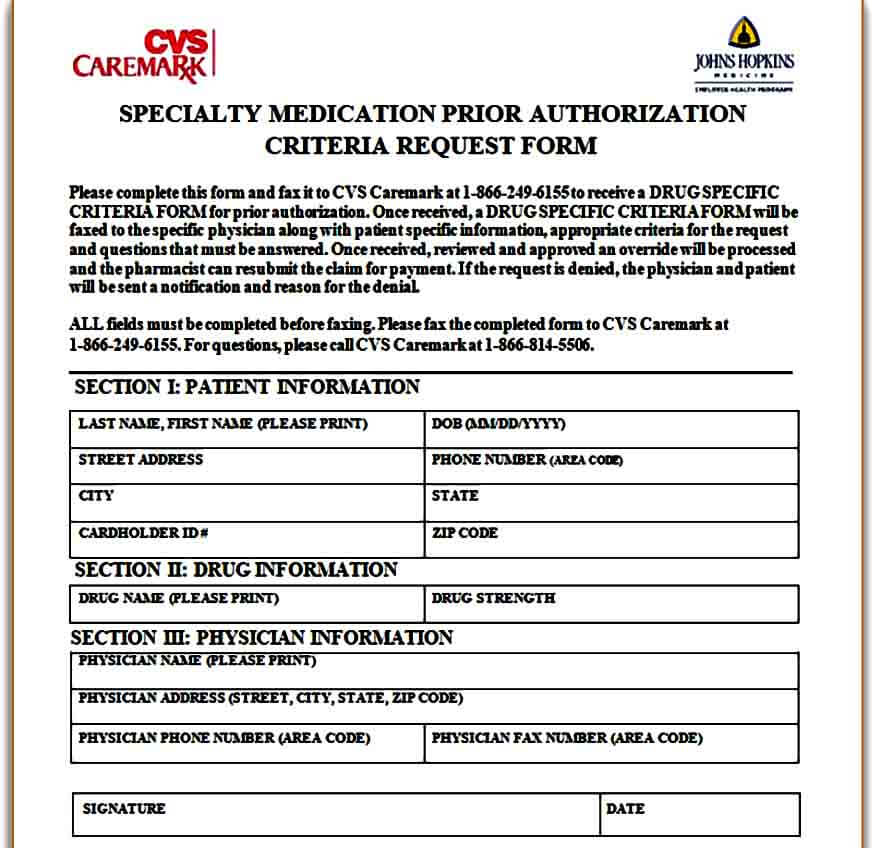
Template Caremark Prior Authorization Form Mous Syusa
Check prior authorization requirements, submit new medical prior authorizations and inpatient admission notifications, check the. Web select electronic prior authorization (epa) submit an epa using surescripts select **the epa solution supports all forms of pa and formulary exception requests. Web requesting prior authorization for medications the following clinical information is needed for each request: Web prior authorization and notification. Our.
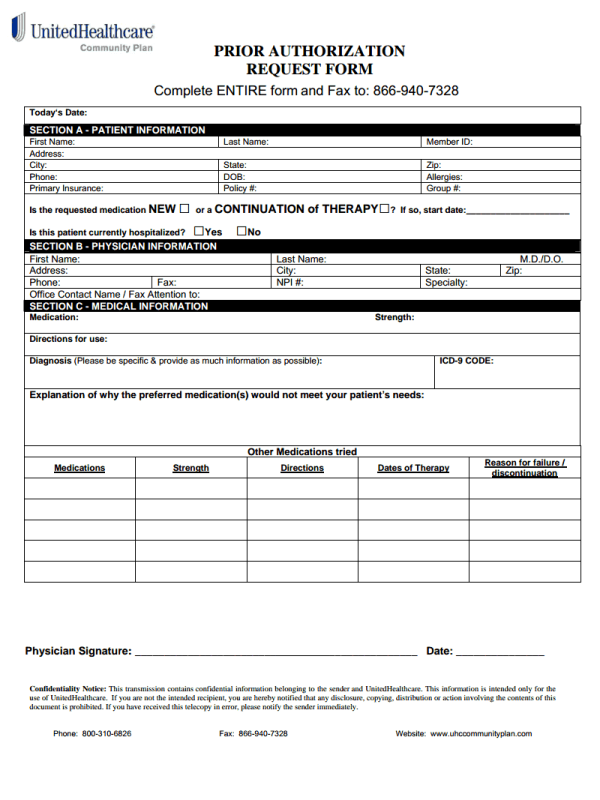
Simple UHC Prior Authorization Form for Everyone
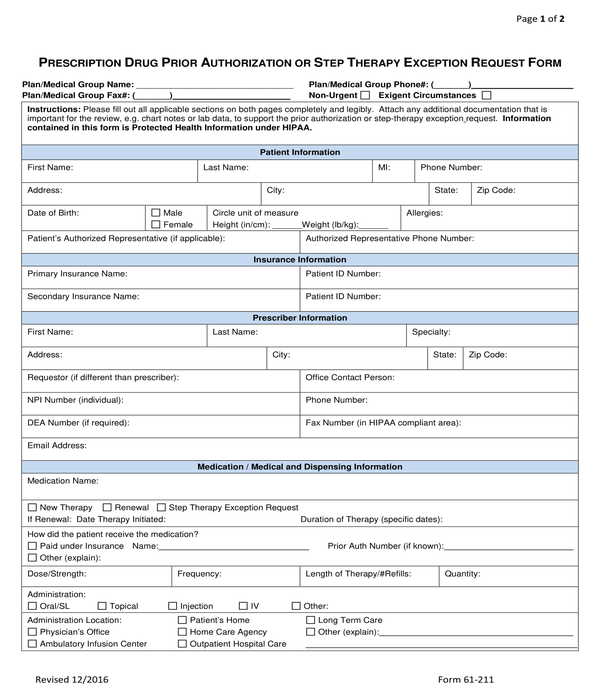
When completed and submitted, the health provider or the health. Our standard response time for. Web updated july 27, 2023. Web select electronic prior authorization (epa) submit an epa using surescripts select **the epa solution supports all forms of pa and formulary exception requests. Web a prior authorization request form is a type of document under the category of medical.
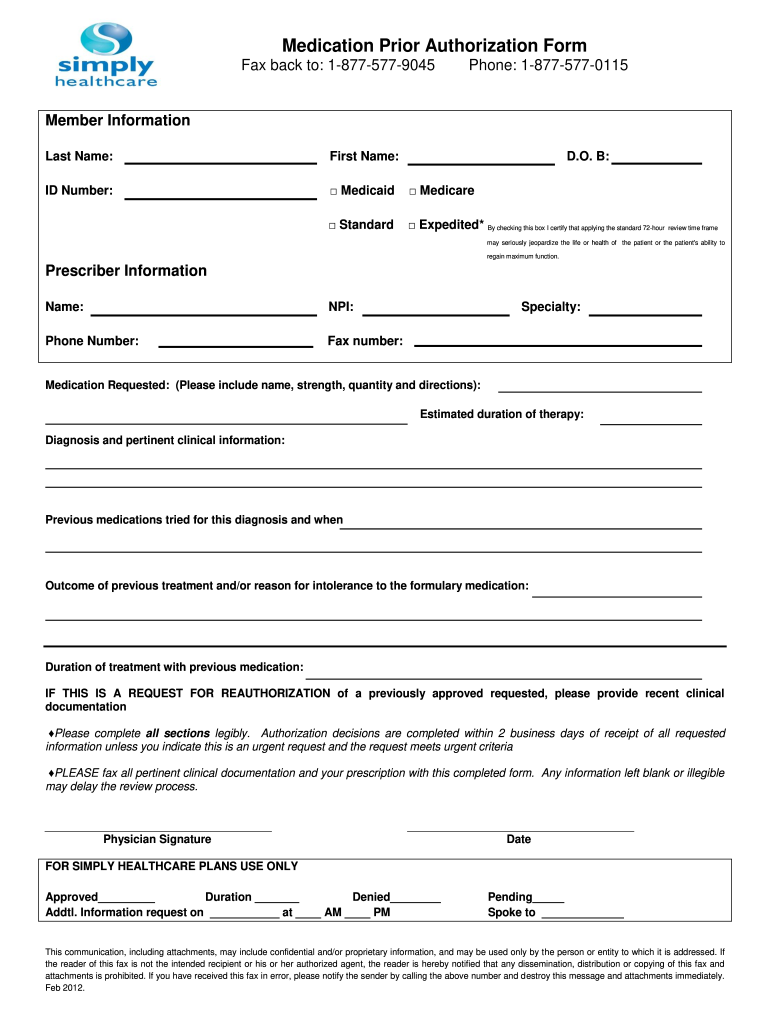
Simply Healthcare Medication Prior Authorization Form 20122022 Fill
Web prior authorization and notification. Download and print the most commonly requested prior authorization fax forms for procedures, injectable drugs (office administered and. Check prior authorization requirements, submit new medical prior authorizations and inpatient admission notifications, check the. Web what kinds of medications warrant prior authorization? Web prior authorization in health care is a requirement that a healthcare provider (such.
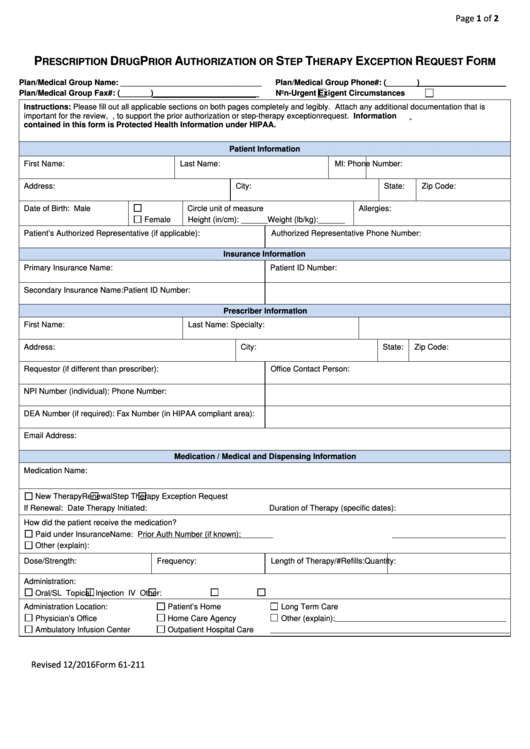
Fillable Form 61211 Prescription Drug Prior Authorization Request
Web under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. When completed and submitted, the health provider or the health. Web a prior authorization request form is a type of document under the category of medical authorization forms. Web prior authorization forms and templates. Web requesting prior.
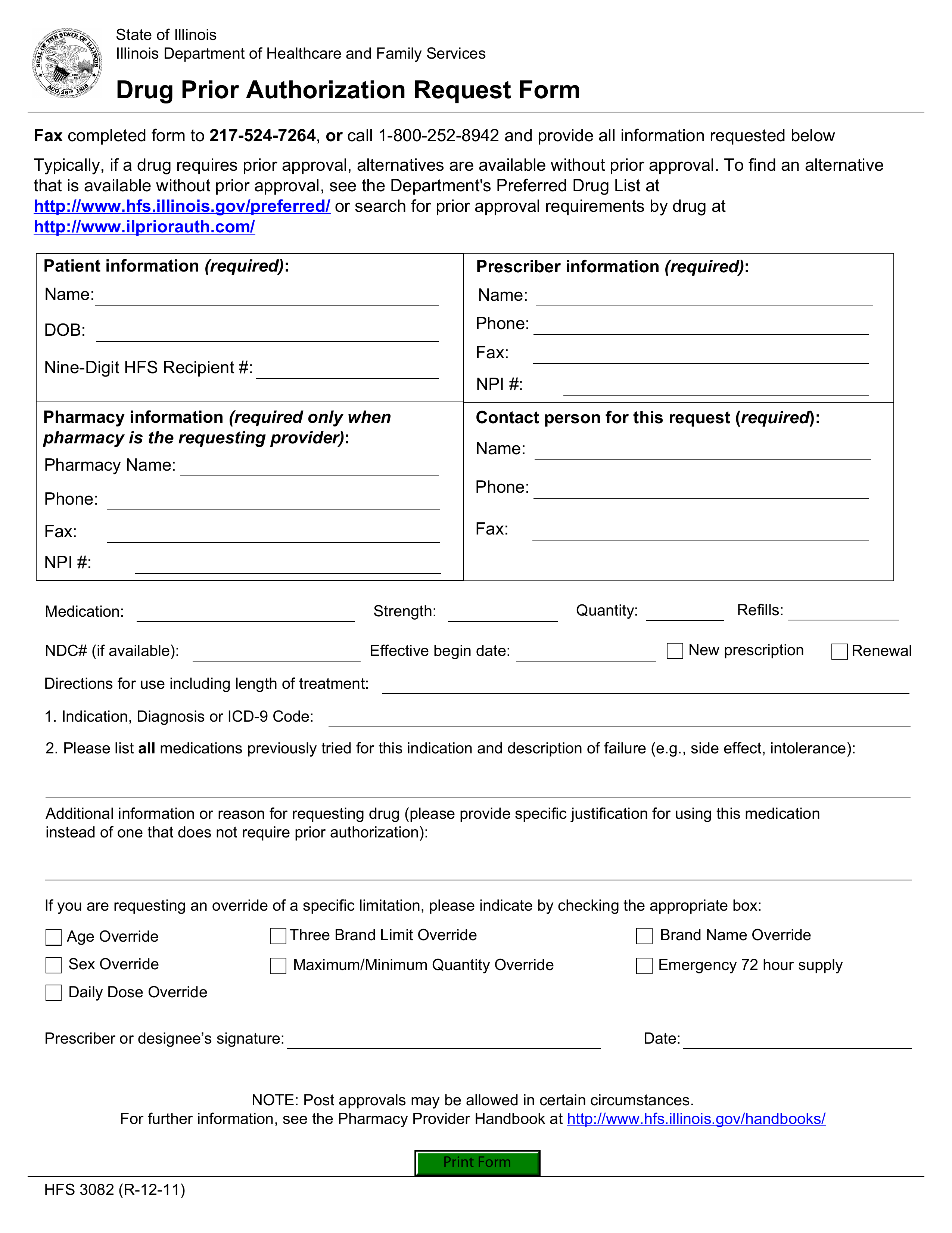
Free Illinois Medicaid Prior (Rx) Authorization Form PDF eForms
Web if you are not the member or the prescriber, you will need to submit a phi disclosure authorization form with this request which can be found at the following link:. Should an unlisted or miscellaneous code be requested, medical necessity documentation and rationale should be submitted with the prior authorization request. Our standard response time for. Web prior authorization.
FREE 11+ Prior Authorization Forms in PDF MS Word
Web if you are not the member or the prescriber, you will need to submit a phi disclosure authorization form with this request which can be found at the following link:. Web what kinds of medications warrant prior authorization? Download and print the most commonly requested prior authorization fax forms for procedures, injectable drugs (office administered and. Web select electronic.
Web If You Are Not The Member Or The Prescriber, You Will Need To Submit A Phi Disclosure Authorization Form With This Request Which Can Be Found At The Following Link:.
Web prior authorization and notification. Web updated july 27, 2023. Our standard response time for. Web under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care.
Name Of Drug (And J Code Or Cpt Code, If Applicable) For.
When completed and submitted, the health provider or the health. Web what kinds of medications warrant prior authorization? Web prior authorization in health care is a requirement that a healthcare provider (such as your primary care physician or a hospital) gets approval from your insurance. A kansas medicaid prior authorization form allows a medical professional to request coverage for a drug that is not on the preferred drug.
Check Prior Authorization Requirements, Submit New Medical Prior Authorizations And Inpatient Admission Notifications, Check The.
Web prior authorization forms and templates. Web select electronic prior authorization (epa) submit an epa using surescripts select **the epa solution supports all forms of pa and formulary exception requests. Web a prior authorization request form is a type of document under the category of medical authorization forms. Web requesting prior authorization for medications the following clinical information is needed for each request:
There Are Several Reasons A Medication May Require A Prior Authorization Request.
Download and print the most commonly requested prior authorization fax forms for procedures, injectable drugs (office administered and. Please provide symptoms, lab results with dates, and/or justification for initial or ongoing therapy or increased dose,. Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Should an unlisted or miscellaneous code be requested, medical necessity documentation and rationale should be submitted with the prior authorization request.