Preferred Care Partners Prior Authorization Form
Preferred Care Partners Prior Authorization Form - A priority partners prior authorization form allows a medical professional to request coverage for a medication that isn’t under the medical. Web includes current vital signs, medications, lab and test results, activity level, therapy notes, consult notes, plan of care, discharge planning (as applicable to the request). Web please use the enterprise precede authorization list (epal) to see what services requisition authorization. Claims inquiry form ( pdf) itemized bill submission form. Simplification of the health care delivery system. Web we improve the health of our members by providing: You may also ask us for a. Web if you are using one of these devices please use the pdf to complete your form. This form allows carepartners of connect medicare advantage hmo and ppo plan members to request dear delivery of. Web this form may be sent to us by mail or fax:
Web we improve the health of our members by providing: If you want to, you can name another person to. Web 2023 optumrx home delivery prescription order form. Web this form may be sent to us by mail or fax: Web optum* manages the skilled nursing provider and facility network for unitedhealthcare. Preferred care network and preferred care. Web if you are using one of these devices please use the pdf to complete your form. Web please use the enterprise precede authorization list (epal) to see what services requisition authorization. Web to request prior authorization, please submit your request online or by phone: Cardiology prior authorization and notification;
Web includes current vital signs, medications, lab and test results, activity level, therapy notes, consult notes, plan of care, discharge planning (as applicable to the request). Web to request prior authorization, please submit your request online or by phone: Web coverage determination and prior authorization request for medicare part b versus part d this form allows physicians to submit information to carepartners of. Use the prior authorization and notification tool on unitedhealthcare. If you have questions, please contact your optum provider advocate, contract manager. Web to access the prior authorization request form, select your state below; Claims inquiry form ( pdf) itemized bill submission form. This form allows carepartners of connect medicare advantage hmo and ppo plan members to request dear delivery of. Simplification of the health care delivery system. Web general information this list contains prior authorization requirements for preferred care network (formerly medica healthcare) and preferred care partners of.
About Privacy Policy Copyright TOS Contact Sitemap
You may also ask us for a. Web forms for submitting prior authorization requests sign in to check the status of your prior authorization claim and select authorizations or referrals from your menu. A priority partners prior authorization form allows a medical professional to request coverage for a medication that isn’t under the medical. Web 2023 optumrx home delivery prescription.
Aarp Prior Authorization Form Form Resume Examples dP9lDOk9RD
If you have questions, please contact your optum provider advocate, contract manager. Web if you are using one of these devices please use the pdf to complete your form. Use the prior authorization and notification tool on unitedhealthcare. Certain services require prior authorization, which results in: A priority partners prior authorization form allows a medical professional to request coverage for.
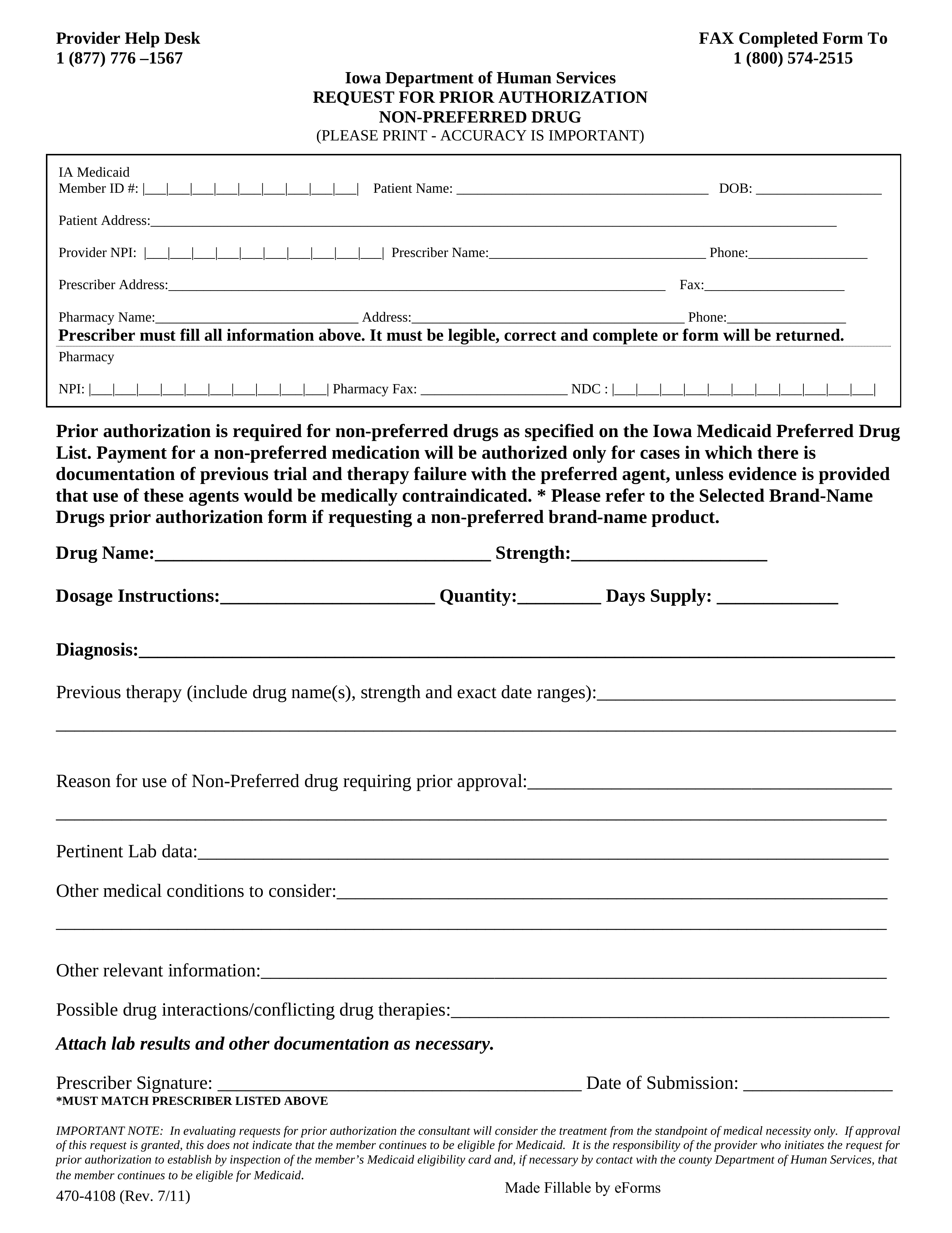
Free Iowa Medicaid Prior (Rx) Authorization Form PDF eForms
If you have questions, please contact your optum provider advocate, contract manager. Web if you are using one of these devices please use the pdf to complete your form. A priority partners prior authorization form allows a medical professional to request coverage for a medication that isn’t under the medical. Web includes current vital signs, medications, lab and test results,.
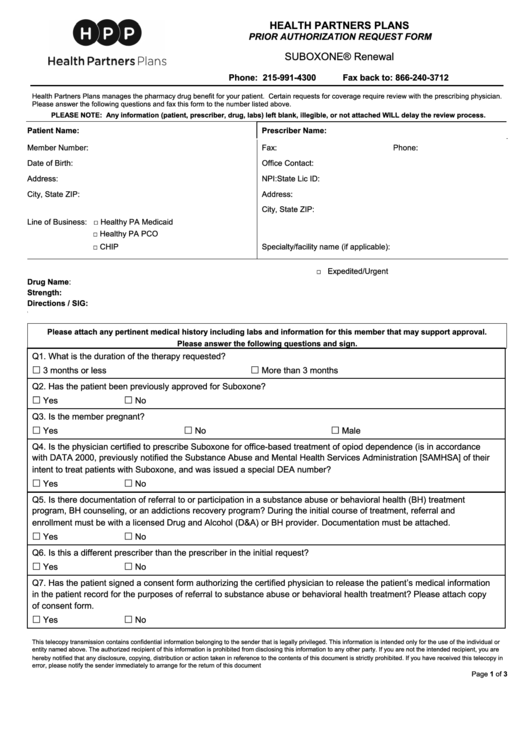
Health Partners Plans Prior Authorization Form
Cardiology prior authorization and notification; Web to access the prior authorization request form, select your state below; Web general information this list contains prior authorization requirements for preferred care network (formerly medica healthcare) and preferred care partners of. Web forms | preferred care partners forms 2023 **appoint a representative you can ask someone to act on your behalf. Web please.
About Privacy Policy Copyright TOS Contact Sitemap
Web this form may be sent to us by mail or fax: Claims inquiry form ( pdf) itemized bill submission form. Certain services require prior authorization, which results in: Web forms | preferred care partners forms 2023 **appoint a representative you can ask someone to act on your behalf. Cardiology prior authorization and notification;
Banner University Family Care Prior Auth Fill Online, Printable
Web we improve the health of our members by providing: Web to request prior authorization, please submit your request online or by phone: Web if you are using one of these devices please use the pdf to complete your form. Medical/dental claim form ( pdf). Simplification of the health care delivery system.
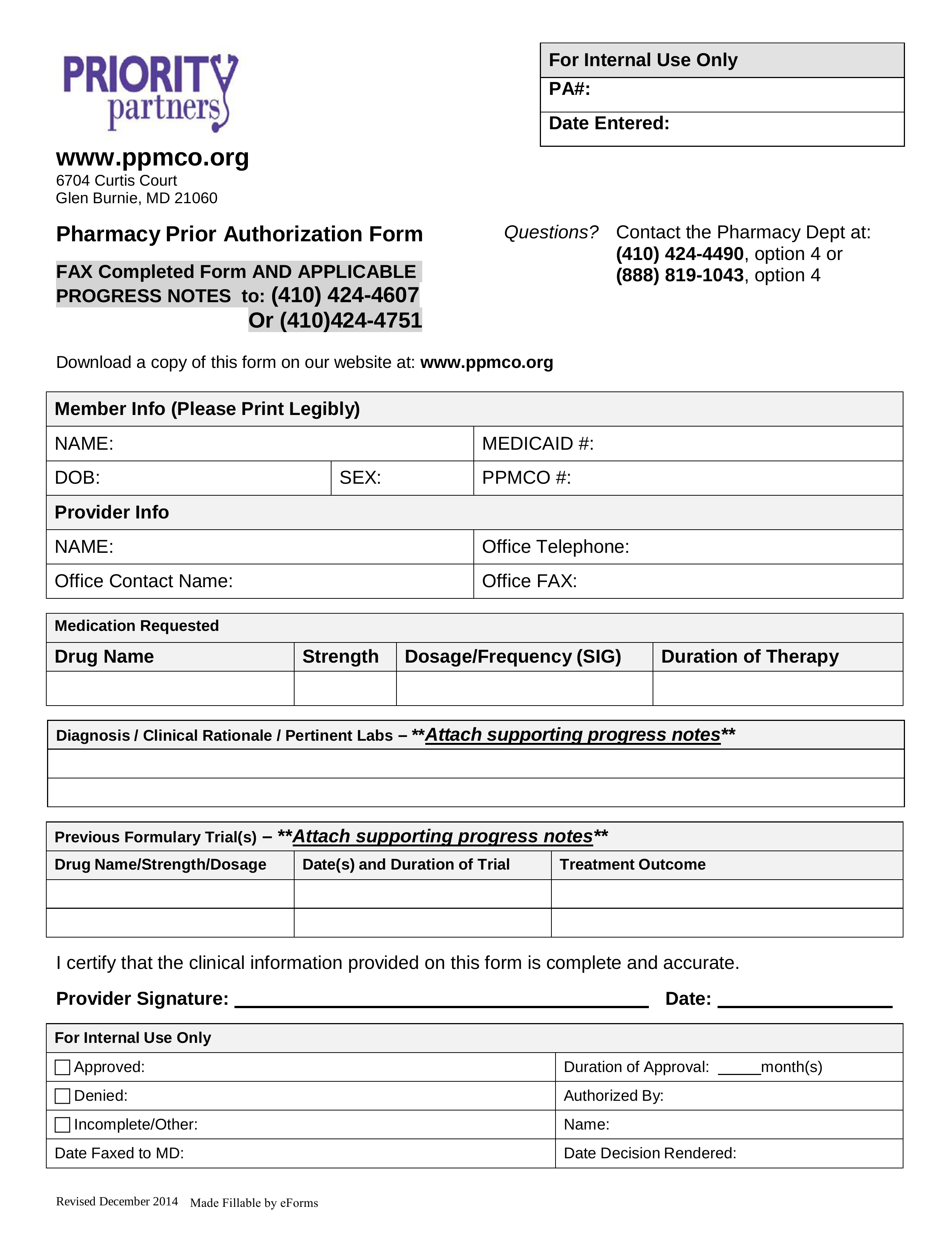
Free Priority Partners Prior (Rx) Authorization Form PDF eForms
This form allows carepartners of connect medicare advantage hmo and ppo plan members to request dear delivery of. Web please use the enterprise precede authorization list (epal) to see what services requisition authorization. Web general information this list contains prior authorization requirements for preferred care network (formerly medica healthcare) and preferred care partners of. Cardiology prior authorization and notification; Claims.
Preferred Care Partners Prior Authorization form 2017 Lovely form Part 347
Medical/dental claim form ( pdf). Web coverage determination and prior authorization request for medicare part b versus part d this form allows physicians to submit information to carepartners of. Certain services require prior authorization, which results in: If you want to, you can name another person to. If you have questions, please contact your optum provider advocate, contract manager.
Preferred Care Partners Prior Authorization form 2017 Best Of top
Radiology prior authorization and notification This form allows carepartners of connect medicare advantage hmo and ppo plan members to request dear delivery of. Web includes current vital signs, medications, lab and test results, activity level, therapy notes, consult notes, plan of care, discharge planning (as applicable to the request). Web to access the prior authorization request form, select your state.
Preferred Care Partners Prior Authorization form 2017 Unique Future
Web to request prior authorization, please submit your request online or by phone: Web this form may be sent to us by mail or fax: Simplification of the health care delivery system. Claims inquiry form ( pdf) itemized bill submission form. Choices for their health care needs.
Certain Services Require Prior Authorization, Which Results In:
Claims inquiry form ( pdf) itemized bill submission form. Preferred care network and preferred care. Choices for their health care needs. Acess to health care services.
Simplification Of The Health Care Delivery System.
You may also ask us for a. Medical/dental claim form ( pdf). Web to access the prior authorization request form, select your state below; Web please use the enterprise precede authorization list (epal) to see what services requisition authorization.
A Priority Partners Prior Authorization Form Allows A Medical Professional To Request Coverage For A Medication That Isn’t Under The Medical.
Web we improve the health of our members by providing: Use the prior authorization and notification tool on unitedhealthcare. Web forms for submitting prior authorization requests sign in to check the status of your prior authorization claim and select authorizations or referrals from your menu. If you want to, you can name another person to.
Web General Information This List Contains Prior Authorization Requirements For Preferred Care Network (Formerly Medica Healthcare) And Preferred Care Partners Of.
Web optum* manages the skilled nursing provider and facility network for unitedhealthcare. Web forms | preferred care partners forms 2023 **appoint a representative you can ask someone to act on your behalf. Web this form may be sent to us by mail or fax: Web includes current vital signs, medications, lab and test results, activity level, therapy notes, consult notes, plan of care, discharge planning (as applicable to the request).