Mental Health Soap Note Template
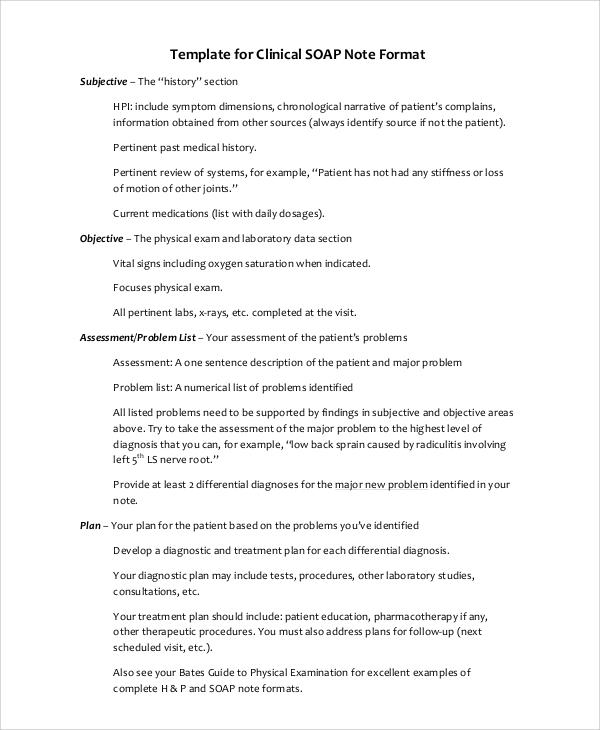
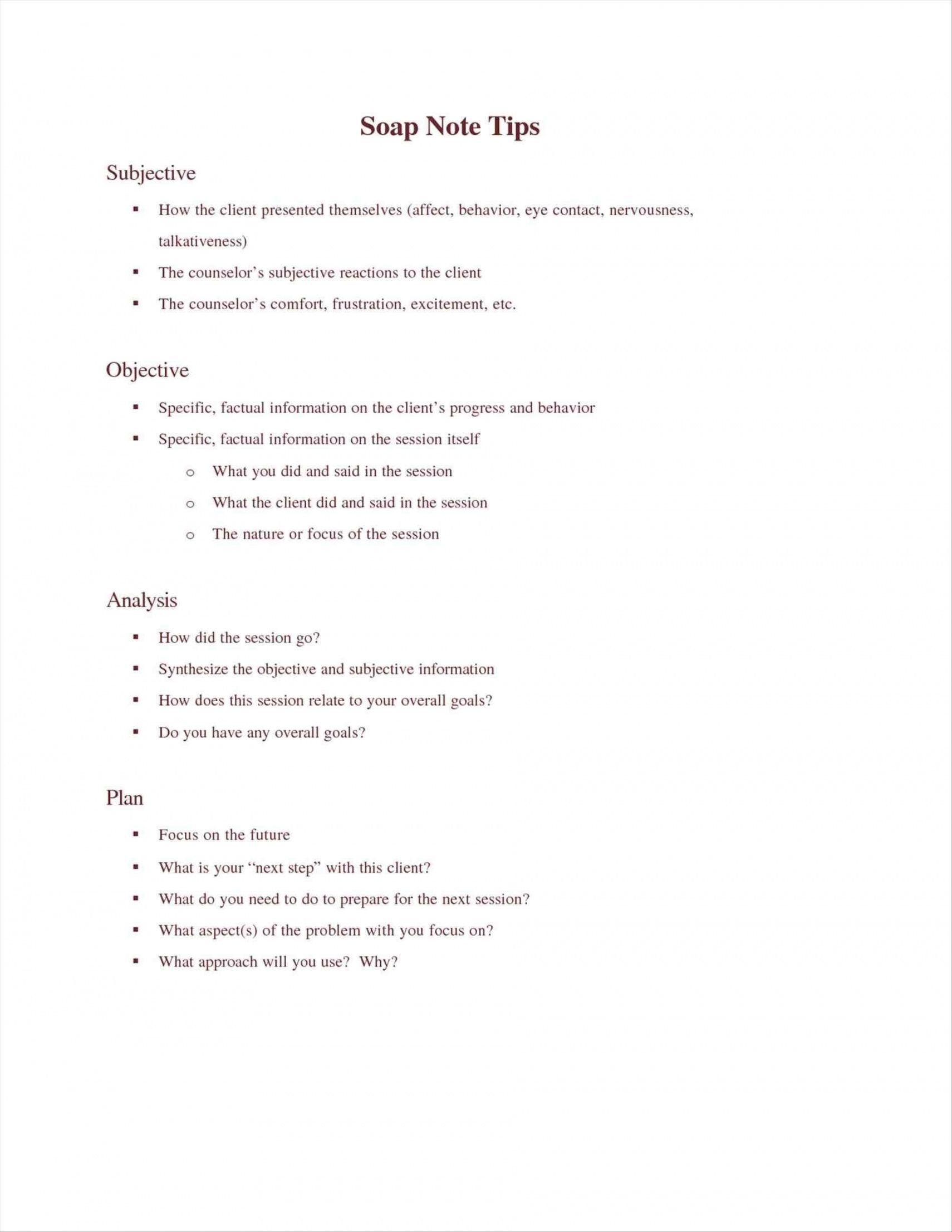
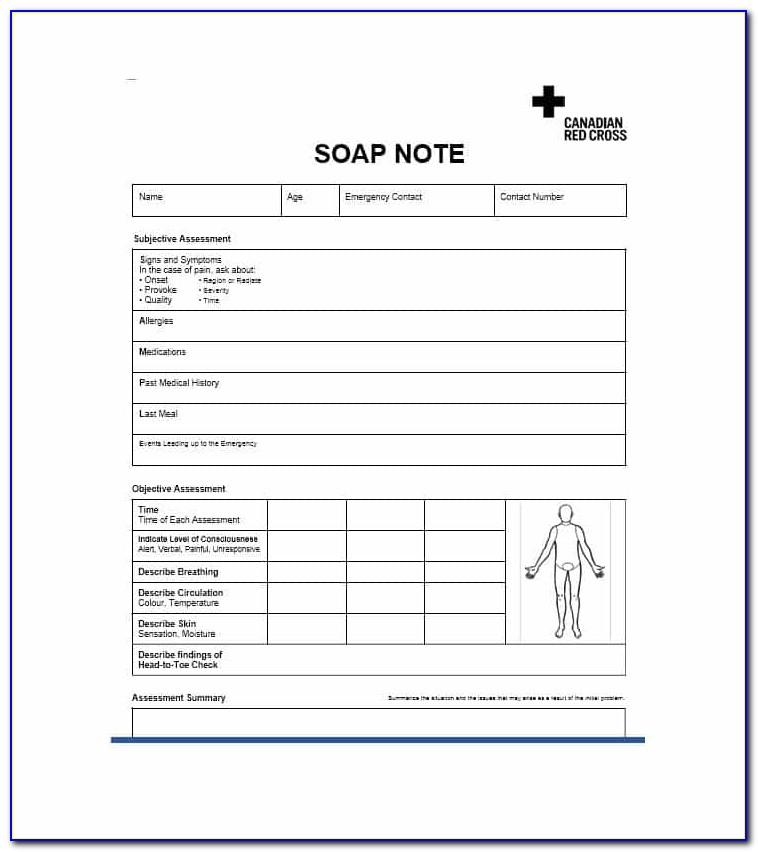
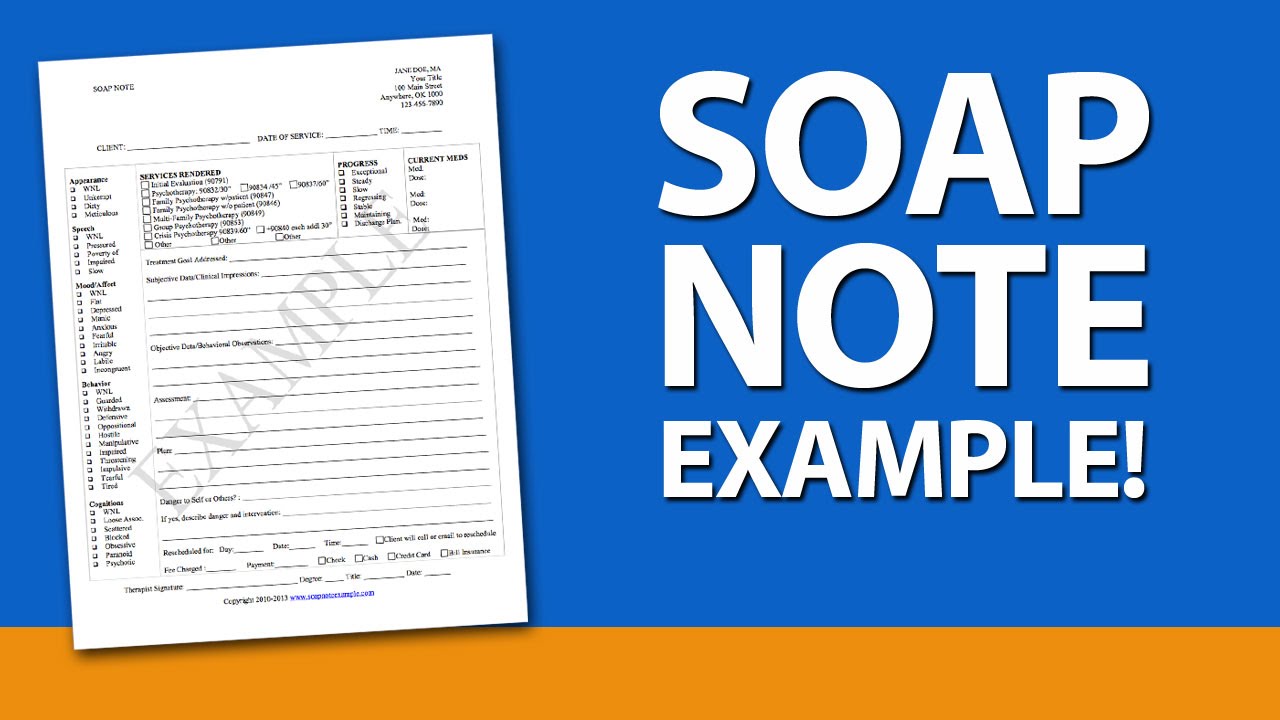
Mental Health Soap Note Template - Subjective, objective, assessment, and plan. Soap note for medical practitioners (care cloud, n.d.): Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Web 3 helpful templates and formats with a solid grasp of the soap acronym, you as a practitioner can improve the informative power of your p rogress notes, as well as the speed with which you write them. Here are three templates you can use for a medical visit, therapy, or coaching session. S = subjective information, such as quotes from the client, or paraphrased statements they’ve given in session. Web how to use this soap note template for mental health. Web mental health progress note templates & examples (2023) mental health progress notes. Web numerous websites offer free soap templates.
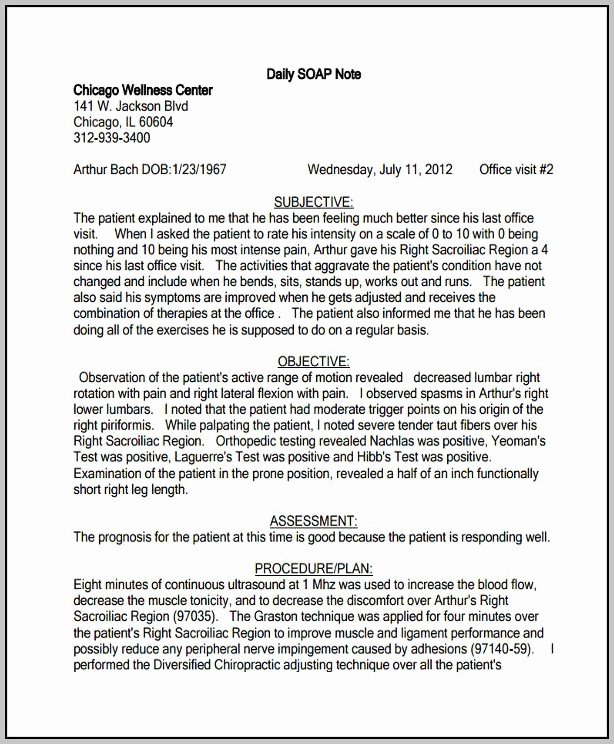
Download our soap notes template pdf file right now. Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Subjective this covers your patient’s detailed medical history and current symptoms. Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Web numerous websites offer free soap templates. Notes from your verbal interaction with patients as well as what they tell you about their condition go here. Web mental health progress note templates & examples (2023) mental health progress notes. Client was tearful during session with a sad affect and required pauses in.
Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Well… as a healthcare professional, remembering details about every session can take a tremendous toll on your mental load (and health 🥴), no matter how good your memory is. Soap note for medical practitioners (care cloud, n.d.): Client was tearful during session with a sad affect and required pauses in. Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Download our soap notes template pdf file right now. And why does everyone keep talking about them? Subjective this covers your patient’s detailed medical history and current symptoms. Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Soap notes are the most common type, containing four separate types of information in four distinct rows:.
FREE 38+ Notes Samples in Google Docs MS Word Apple Pages
Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. And why does everyone keep talking about them? Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Here are three templates you can.
Pin On Counseling Mental Health Soap Note Template Doc IDTcenter
Record your patient’s chief complaint, existing symptoms, and any pain description in this section. S = subjective information, such as quotes from the client, or paraphrased statements they’ve given in session. Subjective, objective, assessment, and plan. Subjective this covers your patient’s detailed medical history and current symptoms. Web numerous websites offer free soap templates.
35 soap Charting Examples Hamiltonplastering
Soap note for medical practitioners (care cloud, n.d.): Download our soap notes template pdf file right now. It’s super easy to use, with the simple layout covering all the bases that you could possibly need when it comes to. Web how to use this soap note template for mental health. Download our comprehensive soap note pdf template for mental health.
Soap Note Template Mental Health Pdf
Health professionals must provide notes that are detailed, succinct, thorough, and simple for other practitioners to use. Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Soap note for medical practitioners (care cloud, n.d.): Download our soap notes template pdf file right now. Download our comprehensive soap.
Soap Note Example Counseling Template 1 Resume Examples edV1y36Vq6
Soap notes are the most common type, containing four separate types of information in four distinct rows:. Web soap notes pdf template for mental health providers. Download our soap notes template pdf file right now. Web how to use this soap note template for mental health. Here are three templates you can use for a medical visit, therapy, or coaching.
SOAP Notes PDF Template and Guide for Mental Health Providers
Subjective, objective, assessment, and plan. Client was tearful during session with a sad affect and required pauses in. Subjective this covers your patient’s detailed medical history and current symptoms. Download our soap notes template pdf file right now. Web 30 blank soap note templates (+examples) march 28, 2021 9 mins read as a health care provider, the records you take.
Soap Note Examples for Mental Health Counselors YouTube
Web 3 helpful templates and formats with a solid grasp of the soap acronym, you as a practitioner can improve the informative power of your p rogress notes, as well as the speed with which you write them. Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage.
62 best List for Notes images on Pinterest Soap note, Hand soaps and
Client was tearful during session with a sad affect and required pauses in. Soap notes cover four important sections: Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Web soap notes pdf template for mental health providers. Subjective this covers your patient’s detailed medical history and current symptoms.
Pin on Sucess Buliding
Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Soap notes are the most common type, containing four separate types of information in four distinct rows:. Soap notes cover four important sections: Web objective identify your observations of the client in today’s session and.
Tips for Writing Better Mental Health SOAP Notes [Updated 2021]
It’s best to choose a few sentences that best represent the most pressing concern your client. Download our soap notes template pdf file right now. Client was tearful during session with a sad affect and required pauses in. Soap notes are the most common type, containing four separate types of information in four distinct rows:. Notes from your verbal interaction.
Web 3 Helpful Templates And Formats With A Solid Grasp Of The Soap Acronym, You As A Practitioner Can Improve The Informative Power Of Your P Rogress Notes, As Well As The Speed With Which You Write Them.
Soap note for medical practitioners (care cloud, n.d.): Web objective identify your observations of the client in today’s session and your factual observations of the client’s progress towards treatment goals. Soap notes cover four important sections: Well… as a healthcare professional, remembering details about every session can take a tremendous toll on your mental load (and health 🥴), no matter how good your memory is.
Notes From Your Verbal Interaction With Patients As Well As What They Tell You About Their Condition Go Here.
Web numerous websites offer free soap templates. Soap notes are the most common type, containing four separate types of information in four distinct rows:. Web 30 blank soap note templates (+examples) march 28, 2021 9 mins read as a health care provider, the records you take decide the level of care that your patients experience. Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes.
It’s Super Easy To Use, With The Simple Layout Covering All The Bases That You Could Possibly Need When It Comes To.
Health professionals must provide notes that are detailed, succinct, thorough, and simple for other practitioners to use. Subjective, objective, assessment, and plan. Subjective this covers your patient’s detailed medical history and current symptoms. Download our soap notes template pdf file right now.
Client Was Tearful During Session With A Sad Affect And Required Pauses In.
Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Web soap notes pdf template for mental health providers. And why does everyone keep talking about them? Record your patient’s chief complaint, existing symptoms, and any pain description in this section.