Express Scripts Tier Exception Form
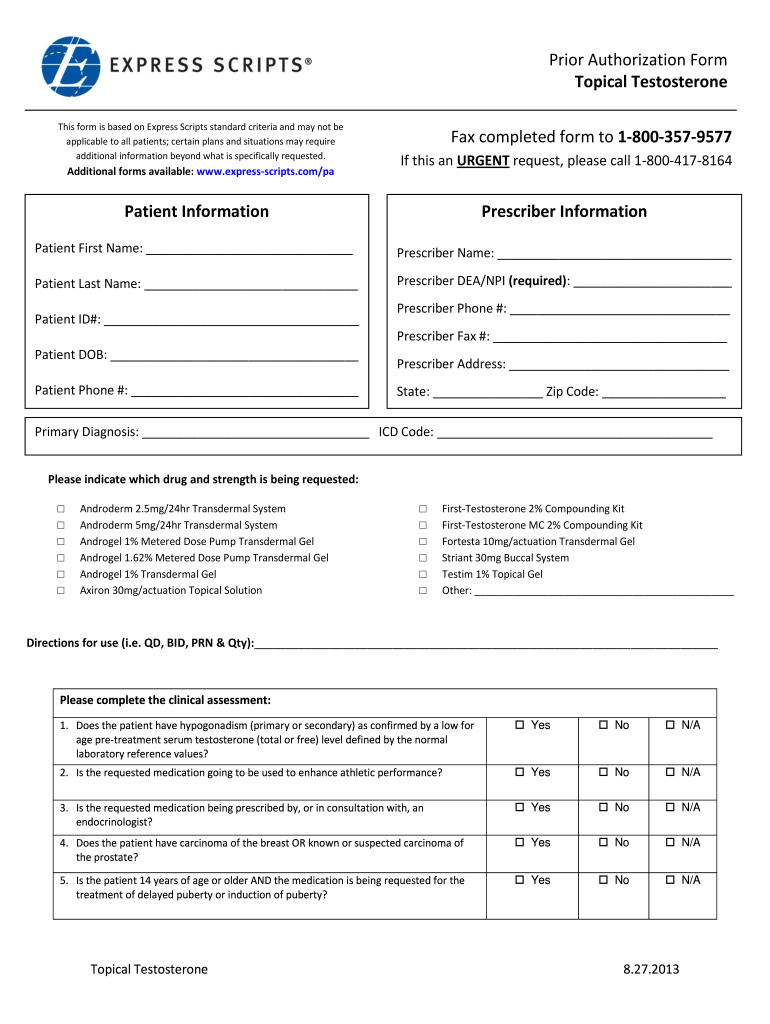
Express Scripts Tier Exception Form - Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains. (1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Web the prescriber can complete a prior authorization electronically or via fax and explain why an exception is required. If you are charged a high copay at the pharmacy, talk to your pharmacist and your plan to find out why. Register now we make it easy to share information get your written prescriptions to us by using our mail order form. Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. You can ask us to make an exception to. Web request for formulary tier exception [specify below:
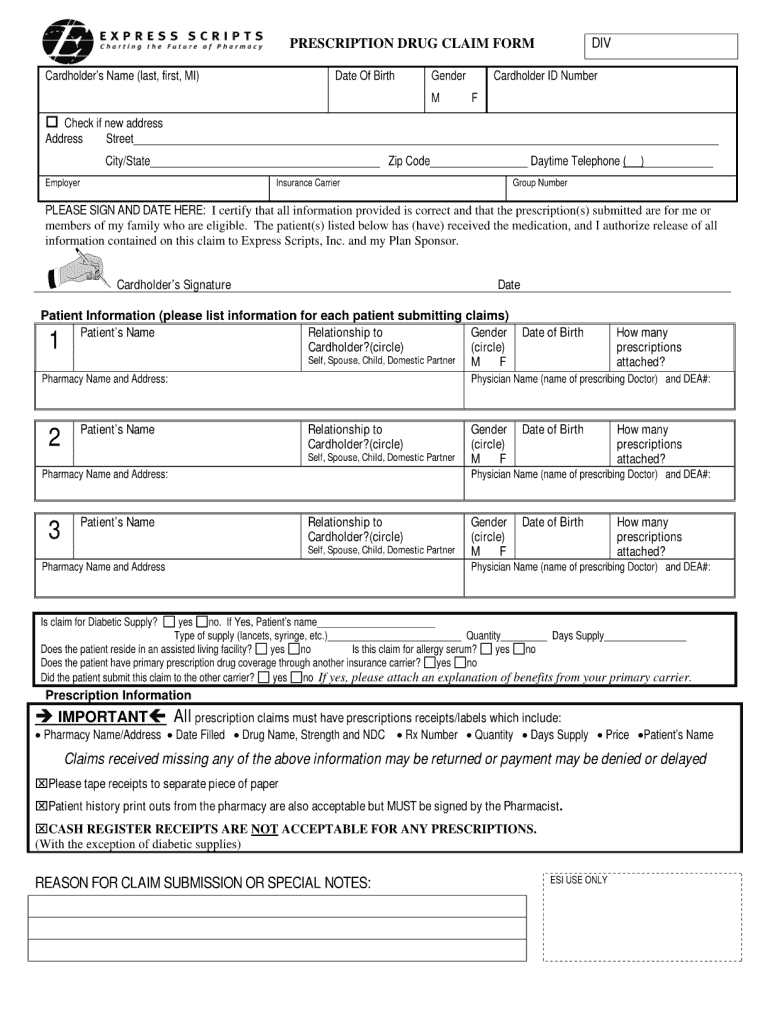
Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Express scripts makes the use of prescription drugs safer and more affordable. Web tier exception coverage determination (for provider use only) drug & prescription information required (please write legibly) drug name:. Web log in don't have an account? Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Complete copa y* (tie it is not necessary exception f ields. Request for a lower co pay (tieri to completed complete ng exceptio n): You can ask us to cover your. Register now we make it easy to share information get your written prescriptions to us by using our mail order form. If a drug has prior authorization (pa) or utilization management (um) requirements, then the pa or.
Web a prescriber supporting statement is required for tier exception requests. Request for a lower co pay (tieri to completed complete ng exceptio n): You can ask us to make an exception to. In most cases, if you fill a prescription for. Web request for formulary tier exception [specify below: Electronic requests can be done through portals such as. Your prescriber may use the attached. Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Express scripts makes the use of prescription drugs safer and more affordable. Register now we make it easy to share information get your written prescriptions to us by using our mail order form.
Care1st Prior Authorization Form
Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains. You can ask us to make an exception to. Web millions trust express scripts for safety, care and convenience. If a drug has prior authorization (pa) or utilization management (um) requirements, then the pa or. Web 2020 national preferred.
ads/responsive.txt Aetna Medicare Tier Exception form Awesome Cigna
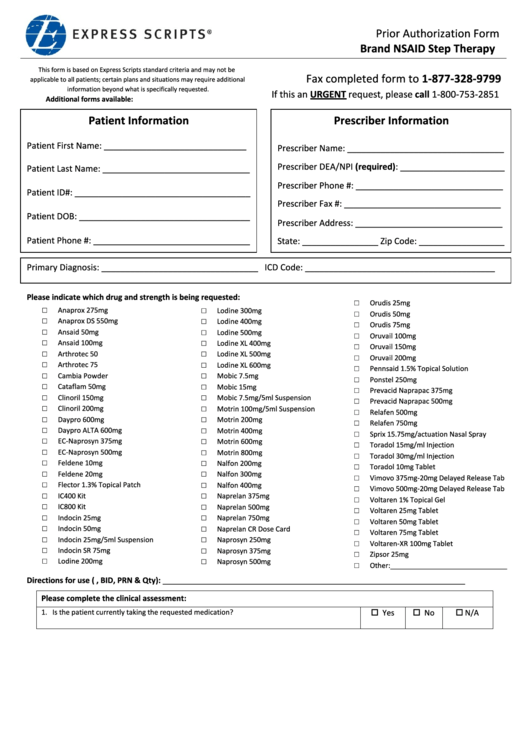
Request for a lower co pay (tieri to completed complete ng exceptio n): Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Web tier.
How to Register for Express Scripts For
Web if the member has tried and failed all the listed drugs or is unable to take the listed drugs for medical reasons, you can submit a formulary exception requesting coverage of the non. Web express scripts is the pharmacy benefit manager for mutual of omaha rx and will be providing this service on behalf of mutual of omaha rx..
Express Scripts Tier Exception Form 2021 Fill Online, Printable
Web express scripts is the pharmacy benefit manager for mutual of omaha rx and will be providing this service on behalf of mutual of omaha rx. Your prescriber may use the attached. Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains. You can ask us to cover your..
ads/responsive.txt Aetna Medicare Tier Exception form Elegant top
Web if the member has tried and failed all the listed drugs or is unable to take the listed drugs for medical reasons, you can submit a formulary exception requesting coverage of the non. If a drug has prior authorization (pa) or utilization management (um) requirements, then the pa or. If you are charged a high copay at the pharmacy,.
Express Scripts Prior Authorization Form Brand Nsaid Step Therapy
Web request for formulary tier exception [specify below: Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Request for a lower co pay (tieri to completed complete ng exceptio n): If a drug has prior authorization (pa) or utilization management (um) requirements,.
Aetna Medicare Tier Exception form Elegant Aco
Web log in don't have an account? In most cases, if you fill a prescription for. Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Register now we make it easy to share information get your written prescriptions to us by using.
Express Scripts Fax Forms for Physicians Prior Authorization Fill Out
Web millions trust express scripts for safety, care and convenience. Web express scripts is the pharmacy benefit manager for mutual of omaha rx and will be providing this service on behalf of mutual of omaha rx. Express scripts makes the use of prescription drugs safer and more affordable. If a drug has prior authorization (pa) or utilization management (um) requirements,.
Optum Rx Prior Authorization Form 11 Thefrenchteeshirt
In most cases, if you fill a prescription for. You can ask us to make an exception to. Electronic requests can be done through portals such as. (1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; Request for a lower co pay (tieri to completed complete ng exceptio n):
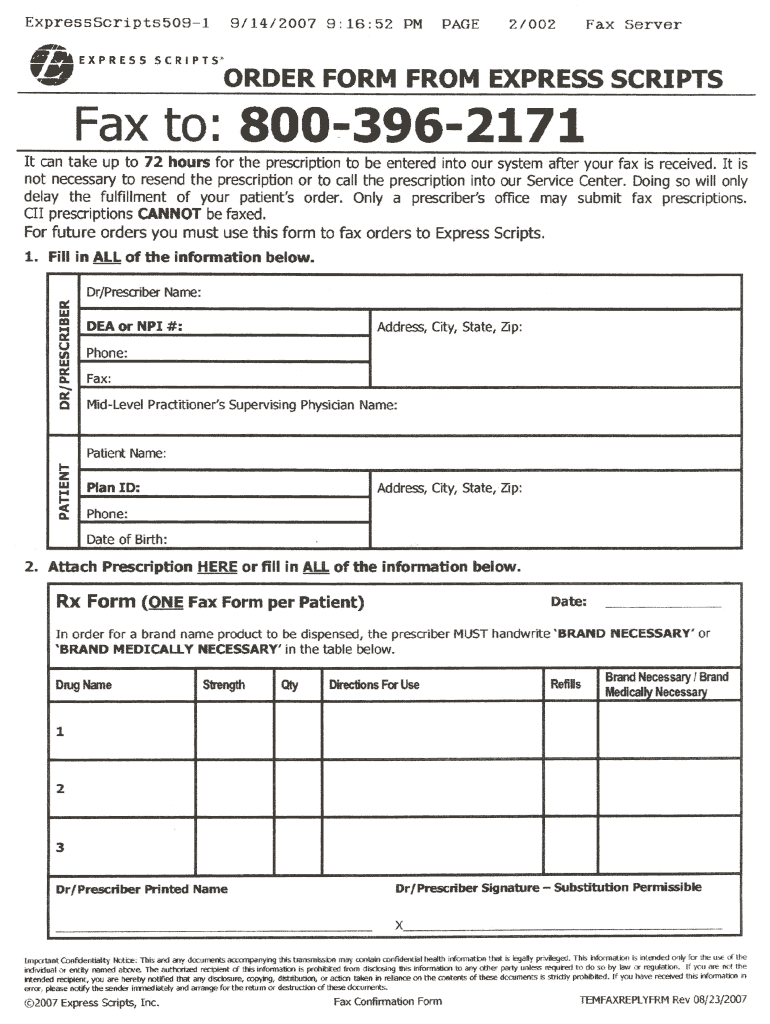
Order Form from Express Scripts 20072021 Fill and Sign Printable
Web a prescriber supporting statement is required for tier exception requests. Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains. In most cases, if you fill a prescription for. Web millions trust express scripts for safety, care and convenience. Your prescriber may use the attached.
Web The Prescriber Can Complete A Prior Authorization Electronically Or Via Fax And Explain Why An Exception Is Required.
Electronic requests can be done through portals such as. Your prescriber may use the attached. If you are charged a high copay at the pharmacy, talk to your pharmacist and your plan to find out why. Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains.
Express Scripts Makes The Use Of Prescription Drugs Safer And More Affordable.
Web if the member has tried and failed all the listed drugs or is unable to take the listed drugs for medical reasons, you can submit a formulary exception requesting coverage of the non. Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. You can ask us to make an exception to. In most cases, if you fill a prescription for.
You Can Ask Us To Cover Your.
Web 2020 national preferred formulary exclusions the excluded medications shown below are not covered on the express scripts drug list. Web follow the steps below when asking for a tiering exception: Register now we make it easy to share information get your written prescriptions to us by using our mail order form. Web tier exception coverage determination (for provider use only) drug & prescription information required (please write legibly) drug name:.
Web A Prescriber Supporting Statement Is Required For Tier Exception Requests.
Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. If a drug has prior authorization (pa) or utilization management (um) requirements, then the pa or. Prior authorization criteria is available upon. Web request for formulary tier exception [specify below: