Express Scripts Appeal Form Non Medicare
Express Scripts Appeal Form Non Medicare - Click here to get started. Web request an appeal what’s the form called? Web because we, express scripts, denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us for a redetermination (appeal) of our. Express scripts or rdt will respond in writing to you and/or your physician with a letter explaining the outcome of the appeal. Web express scripts manages your prescription drug benefit at the request of your health plan. We have received your pricing inquiry. Web your appeal must: Web epa is the preferred method to submit prior authorization requests to express scripts for pharmacy benefit drugs. Pharmacist resource center pricing inquiry received thank you for contacting express scripts pharmacy services. Use this contact information if you need to file an appeal if your coverage review is denied.
Pharmacist resource center pricing inquiry received thank you for contacting express scripts pharmacy services. We have received your pricing inquiry. Web clinical and administrative appeals. Web to initiate the coverage review process or an appeal of a previously declined coverage review request, please use the resources below: Web express scripts resources for pharmacists. Web initial coverage review purpose: Web now is a great time for you to make the switch to electronic prior authorization (epa). You recentlycontacted us to request coverage beyond your plan’s standard benefit. Easier to use for prescribers, nurses and office. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and;
Web members include those who have express scripts prescription benefits through their employer, health plan, or directly via medicare part d. Web express scriptsapplication for second level appeal: Read latest notifications, file pricing appeals and search express scripts claims and patient coverage for your pharmacy customers. Web mail your request with the above information to: Faster to send and get reviews. Web an appeal, or redetermination, is a formal way to ask the plan to review a coverage decision about health care services and/or prescription drugs. Requesting an appeal (redetermination) if you disagree with. Web because we, express scripts, denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us for a redetermination (appeal) of our. Easier to use for prescribers, nurses and office. Web express scripts offers epa options.
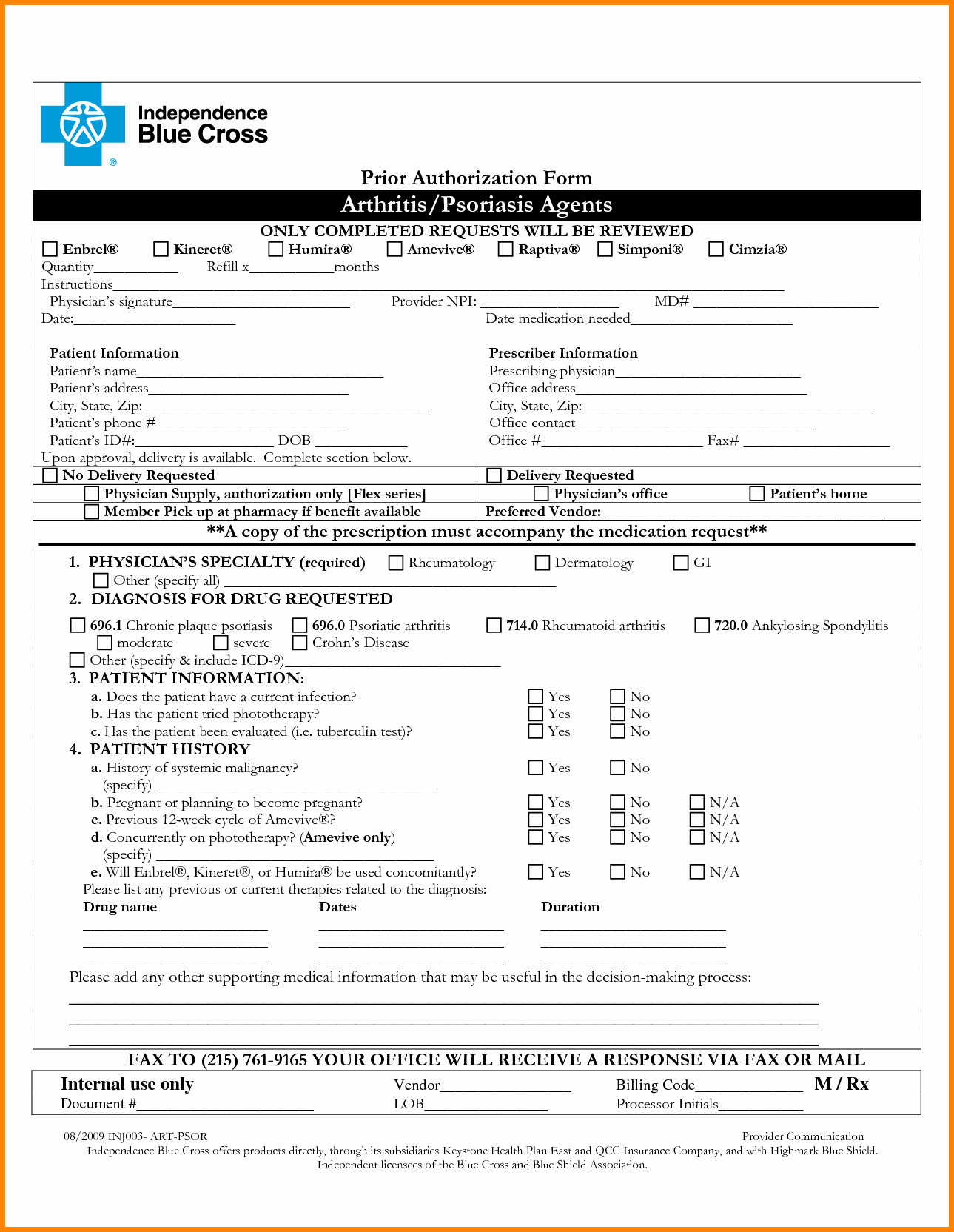
Express Scripts Prior Auth Form Unique Humana Prior
Click here to get started. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; Pharmacist resource center pricing inquiry received thank you for contacting express scripts pharmacy services. Web clinical and administrative appeals. Depending on your plan, you may.
Understanding Your Part D Explanation of Benefits Roadmap For Medicare
Pharmacist resource center pricing inquiry received thank you for contacting express scripts pharmacy services. Providers may use epa through. You recentlycontacted us to request coverage beyond your plan’s standard benefit. We have received your pricing inquiry. Web because we, express scripts, denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us.
True Scripts Prior Authorization form New Express Scripts Prior
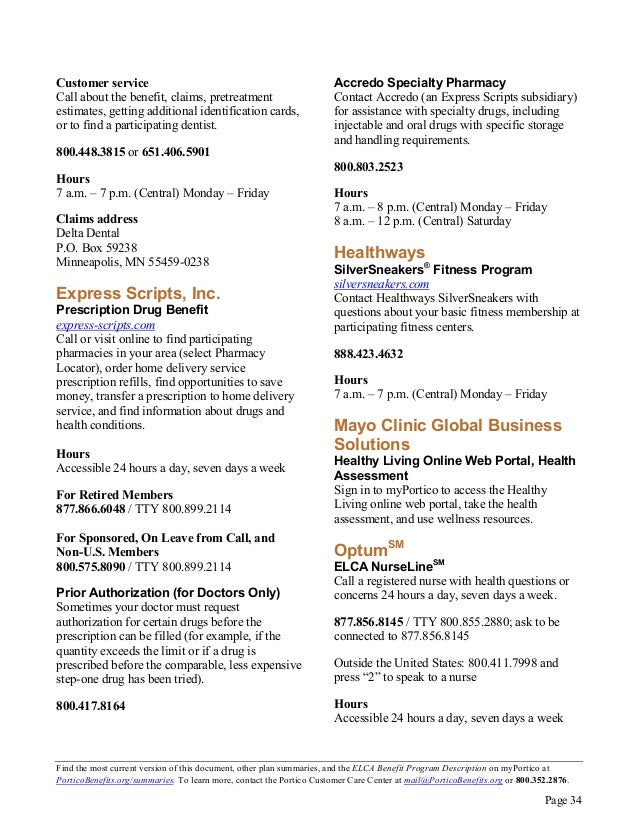
Web members include those who have express scripts prescription benefits through their employer, health plan, or directly via medicare part d. Use this contact information if you need to file an appeal if your coverage review is denied. Web epa is the preferred method to submit prior authorization requests to express scripts for pharmacy benefit drugs. Web mail your request.
57 HQ Images Express Scripts Appeal Form Express Scripts Prior
Pharmacist resource center pricing inquiry received thank you for contacting express scripts pharmacy services. Web an appeal, or redetermination, is a formal way to ask the plan to review a coverage decision about health care services and/or prescription drugs. Web epa is the preferred method to submit prior authorization requests to express scripts for pharmacy benefit drugs. Easier to use.
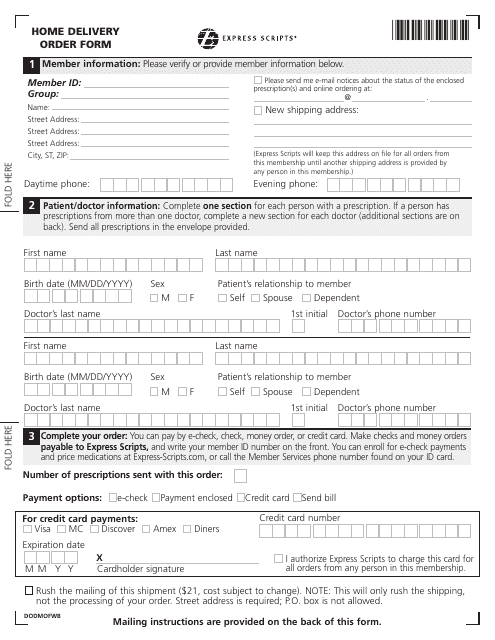
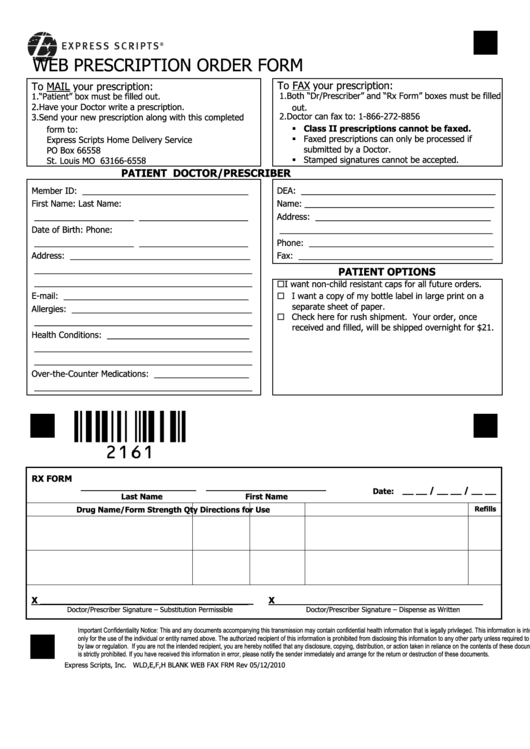
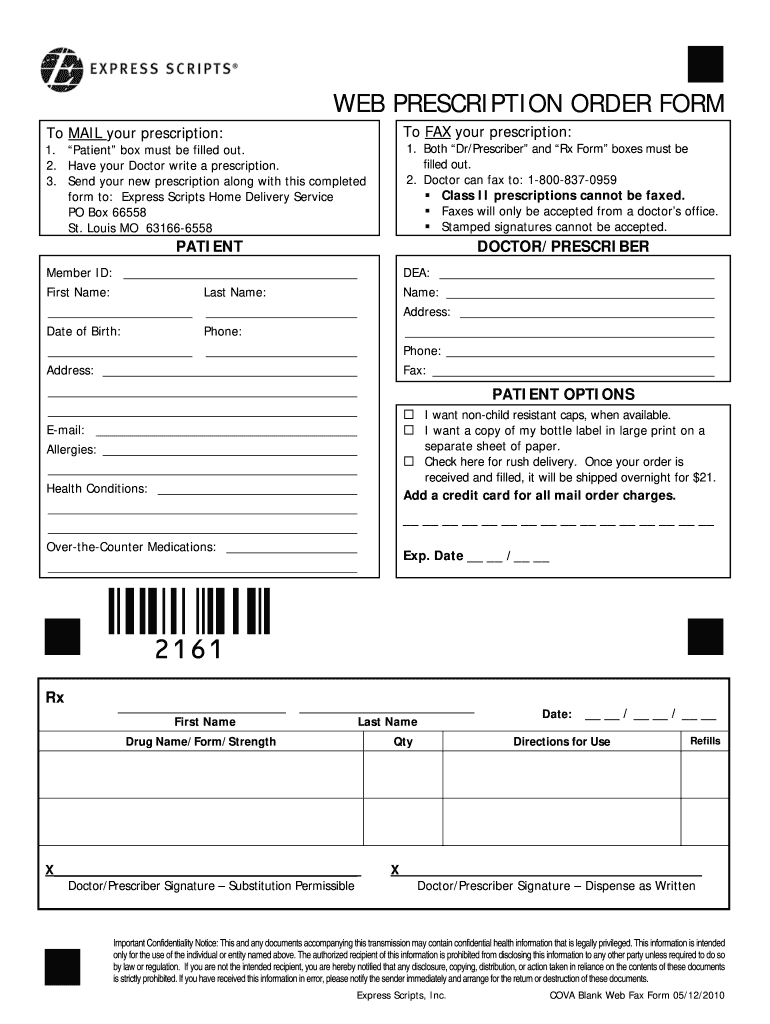
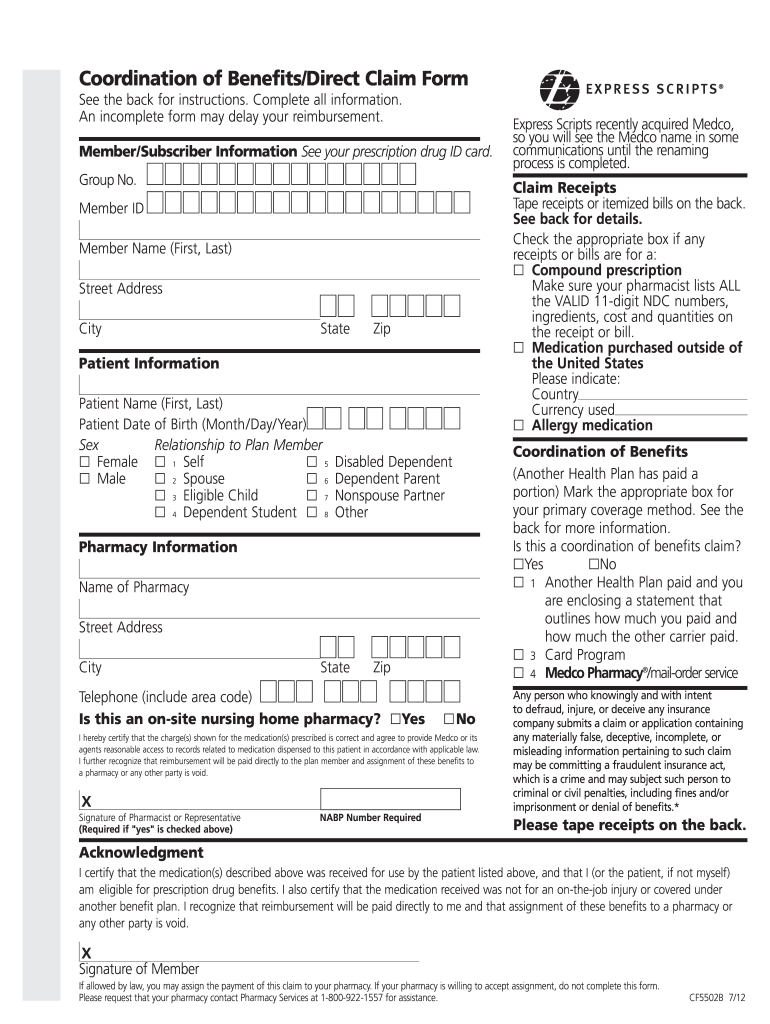
Top 16 Express Scripts Forms And Templates free to download in PDF format
Providers may use epa through. Web your appeal must: Web express scripts resources for pharmacists. Web express scripts manages your prescription drug benefit at the request of your health plan. We have received your pricing inquiry.
Express Scripts Fax Form Fill and Sign Printable Template Online US
Providers may use epa through. Web express scriptsapplication for second level appeal: Requesting an appeal (redetermination) if you disagree with. General express scripts request form (pdf) if you are a minnesota physician, please submit. We have received your pricing inquiry.
Express Scripts Appeal Form Fill Out and Sign Printable PDF Template
Web your appeal must: Web express scripts resources for pharmacists. Web initial coverage review purpose: Web to initiate the coverage review process or an appeal of a previously declined coverage review request, please use the resources below: Use this contact information if you need to file an appeal if your coverage review is denied.
57 HQ Images Express Scripts Appeal Form Express Scripts Prior
Be postmarked or received by. Web express scripts offers epa options. Providers may use epa through. Web clinical and administrative appeals. Web your appeal must:
Silver Scripts Prior Auth Form amulette
Depending on your plan, you may. Web mail your request with the above information to: Web because we, express scripts, denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us for a redetermination (appeal) of our. Web express scripts manages your prescription drug benefit at the request of your health plan..
Vizio Class Action Lawsuit Claim Form Express Scripts Claims Address
You recentlycontacted us to request coverage beyond your plan’s standard benefit. Be postmarked or received by. Faster to send and get reviews. General express scripts request form (pdf) if you are a minnesota physician, please submit. Web epa is the preferred method to submit prior authorization requests to express scripts for pharmacy benefit drugs.
You May Ask For A Review When You.
Requesting an appeal (redetermination) if you disagree with. Web an appeal, or redetermination, is a formal way to ask the plan to review a coverage decision about health care services and/or prescription drugs. You recentlycontacted us to request coverage beyond your plan’s standard benefit. Easier to use for prescribers, nurses and office.
Web Request An Appeal What’s The Form Called?
General express scripts request form (pdf) if you are a minnesota physician, please submit. Click here to get started. Express scripts or rdt will respond in writing to you and/or your physician with a letter explaining the outcome of the appeal. Web express scripts offers epa options.
Be In Writing And Signed, State Specifically Why You Disagree, Include A Copy Of The Claim Decision, And;
Use this contact information if you need to file an appeal if your coverage review is denied. Web because we, express scripts, denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us for a redetermination (appeal) of our. Web clinical and administrative appeals. Depending on your plan, you may.
Web Express Scriptsapplication For Second Level Appeal:
Web now is a great time for you to make the switch to electronic prior authorization (epa). Web express scripts 1.877.328.9799 attn: Be postmarked or received by. Faster to send and get reviews.