Bcbs Provider Appeal Form
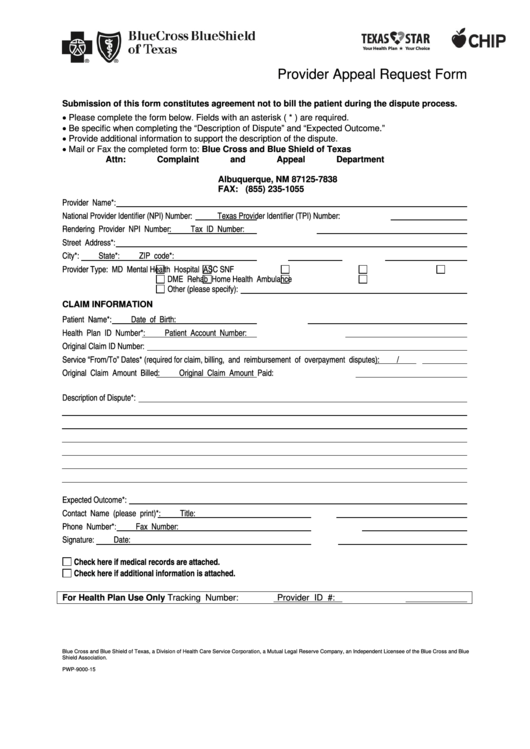
Bcbs Provider Appeal Form - Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! As part of the process, you'll have to fill out the above form. Most provider appeal requests are related to a length of stay or treatment setting denial. Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. Web use this form to submit appeal requests for their commercial and bluecare patients. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Please submit only one claim adjustment, status check or appeal per page and mail with appropriate attachments to blue cross. Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need. If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process.
Web provider forms & guides. Most provider appeal requests are related to a length of stay or treatment setting denial. Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Check the “utilization management” box under appeal type; If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. Be specific when completing the “description of appeal” and “expected outcome.” please provider all supporting documents with submitted appeal. You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”;
Fields with an asterisk (*) are required. Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Please submit only one claim adjustment, status check or appeal per page and mail with appropriate attachments to blue cross. Access and download these helpful bcbstx health care provider forms. This is different from the request for claim review request process outlined above. Web provider forms & guides. And enter the authorization or precertification number. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”;
TN BCBS 17PED153727 20172021 Fill and Sign Printable Template Online
If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Be specific when completing the “description of appeal” and “expected outcome.” please provider all supporting documents with submitted appeal. Web provider appeal request form provider appeal request form please complete one form per member to.
VT BCBS PA.PC.RR 20122021 Fill and Sign Printable Template Online
If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. Web appeal form who is this for? Be specific when completing the “description of appeal” and “expected outcome.” please provider all supporting documents with submitted appeal. This is different from the request.
BCBS in Provider Dispute Resolution Request Form Blue Cross Blue
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! And enter the authorization or precertification number. Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need. Web provider claim adjustment / status check / appeal.
Bcbs Federal Provider Appeal form New Blue Cross Of Mass Giving Opioid
Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need. Access and download these helpful bcbstx health care provider forms. And enter the authorization or precertification number. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal.
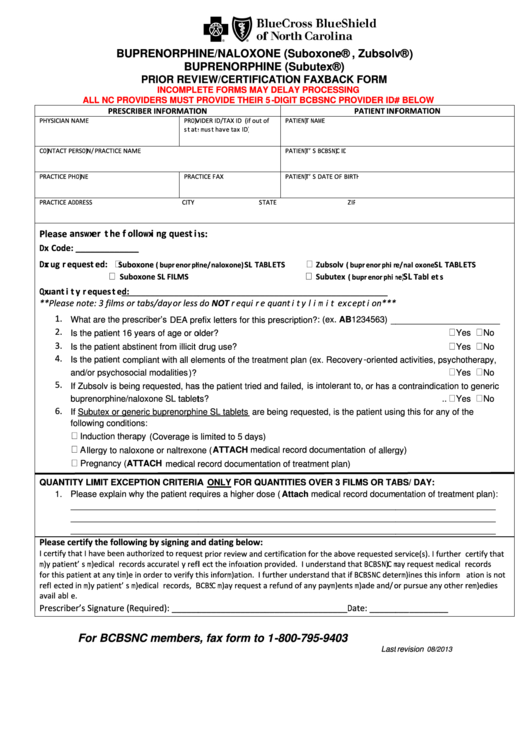
Bcbsnc Prior Review/certification Faxback Form printable pdf download
And enter the authorization or precertification number. Access and download these helpful bcbstx health care provider forms. Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. If you have a problem with your blue cross blue shield of michigan service, you can use.
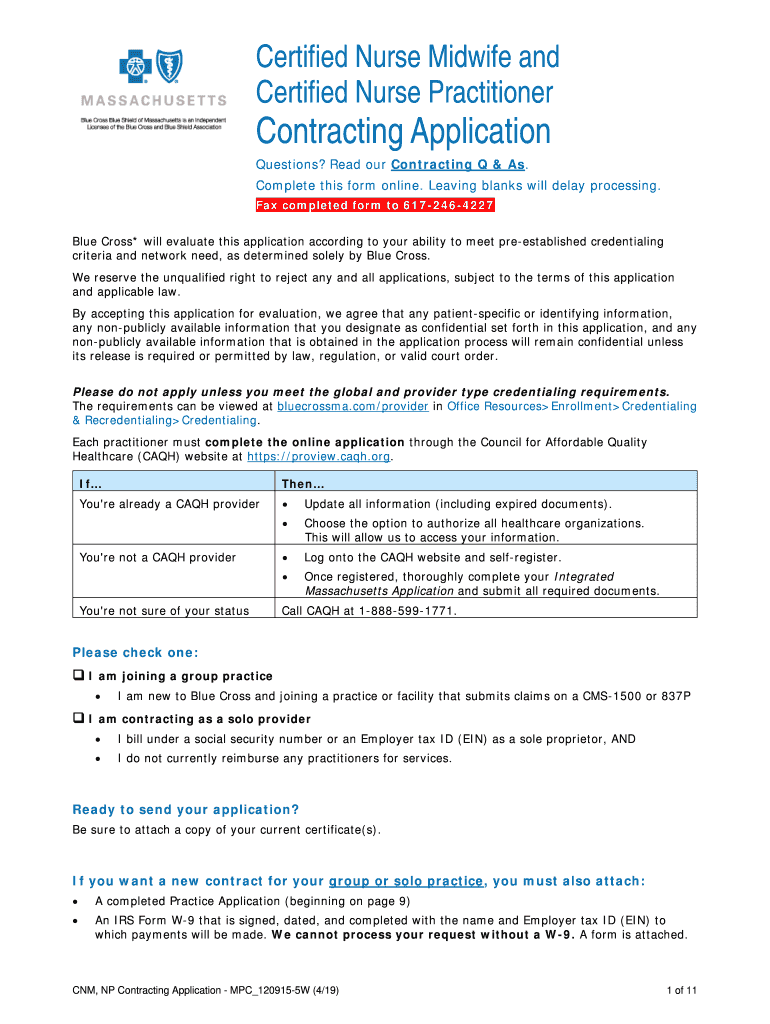
MA BCBS MPC_1209155W 20202021 Fill and Sign Printable Template
Web provider forms & guides. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Check the “utilization management” box under appeal type; Easily find and download forms, guides, and other related documentation that you need to.
Bcbs Federal Provider Appeal form Best Of File Plaint Blue Shield
Web use this form to submit appeal requests for their commercial and bluecare patients. Web appeal form who is this for? Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. Fields with an asterisk (*) are required. And enter the authorization or precertification.
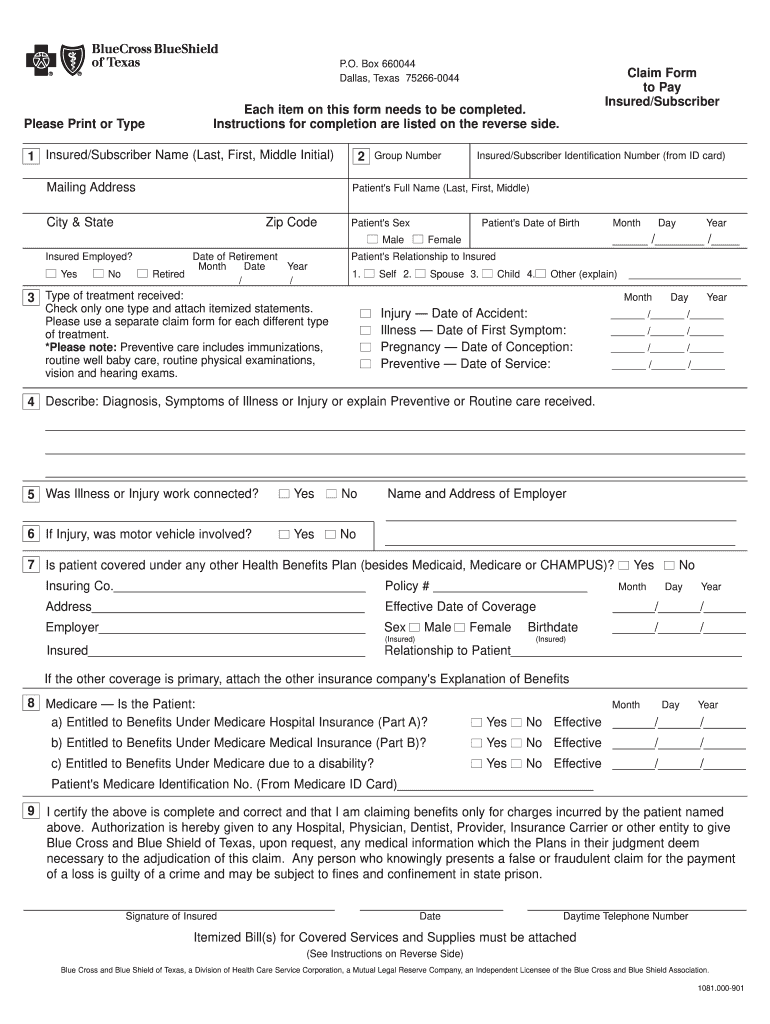
Bcbs Claim Form Fill Out and Sign Printable PDF Template signNow
Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need. Web appeal form who is this for? Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Web provider claim adjustment / status check / appeal.
Texas Bcbs Provider Appeal Fill Out and Sign Printable PDF Template
You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. Web appeal form who is this for? Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Check.
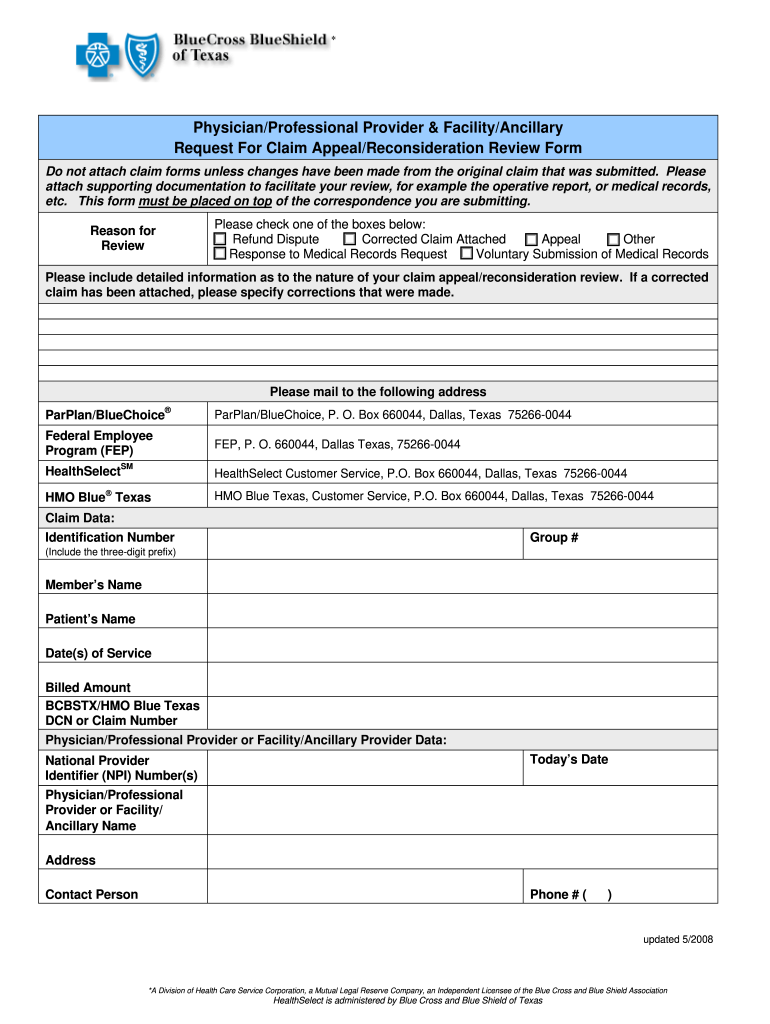
Bluecross Blueshield Of Texas Provider Appeal Request Form printable
Web provider forms & guides. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”; If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. You can find this and the other requirements for an appeal at the centers for medicare.
As Part Of The Process, You'll Have To Fill Out The Above Form.
Access and download these helpful bcbstx health care provider forms. Web provider appeal request form provider appeal request form please complete one form per member to request an appeal of an adjudicated/paid claim. Check the “utilization management” box under appeal type; Most provider appeal requests are related to a length of stay or treatment setting denial.
Web Provider Forms & Guides.
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Web appeal form who is this for? You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us.
Fields With An Asterisk (*) Are Required.
If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. This is different from the request for claim review request process outlined above.
Web Provider Claim Adjustment / Status Check / Appeal Form Instructions Blue Cross Blue Shield Of Minnesota And Blue Plus The General Instructions Are Listed Below.
Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Web use this form to submit appeal requests for their commercial and bluecare patients. Please submit only one claim adjustment, status check or appeal per page and mail with appropriate attachments to blue cross. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”;